Watchful Waiting: Well Behaved Breast Cancers Non-Surgical Management of Breast Cancer
Willis Maurice, Robinson Angelica, Hermann Stephan and Sadruddin Sarfaraz
DOI10.21767/2572-309X.100002
Department of Internal Medicine, UTMB Hematology/Oncology, Dickinson, USA
- *Corresponding Author:
- Maurice Willis
Department of Internal Medicine, UTMB Hematology/Oncology, Dickinson, USA.
Tel: 2815348380
Fax: 2815348399
E-mail: mawillis@utmb.edu
Received date: December 18, 2015; Accepted date: December 28, 2015; Published date: January 04,2016
Citation: Maurice W, Angelica R, Stephan H,et al. Watchful Waiting: Well Behaved Breast Cancers Non-Surgical Management of Breast Cancer. J Adenocarcinoma. 2016, 1:1. doi: 10.21767/2572-309X.10002
Abstract
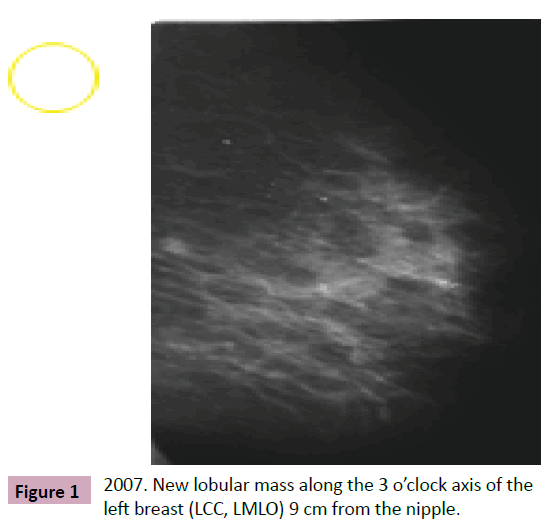
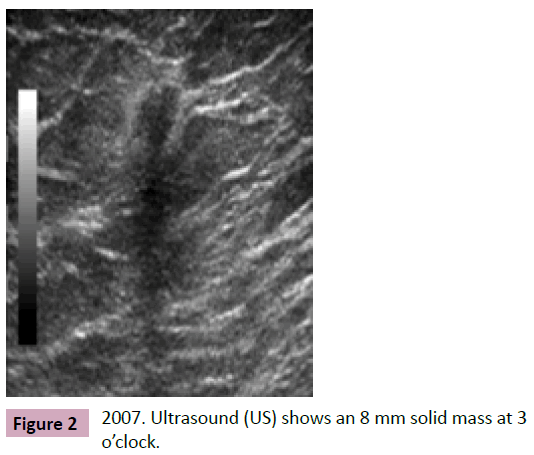
In December 2007, a 71 year old female with no family history of breast cancer had a screening mammogram showing a new subcentimeter mass along the 3 o’clock axis of the left breast, posterior depth. Follow up ultrasound in February of 2008 showed an 8 mm solid mass at 3 o'clock, 9 cm from the nipple, which correlated with the mammographic mass. Ultrasound of the axilla was unremarkable. Biopsy of the mass showed: moderately differentiated invasive ductal carcinoma, grade 2, ER+ (90%), PR+ (50%), her2neu- (1+), Ki-67 10% (low proliferative rate). The patient was referred to surgical oncology, radiation oncology, and medical oncology for consultation; however, she declined any surgical intervention or radiation therapy. Furthermore, the patient stated that she was only willing to take oral therapy, so aromatase inhibitors were thoroughly discussed with the patient including the side effects of osteoporosis.
Case 1
In December 2007, a 71 year old female with no family history of breast cancer had a screening mammogram showing a new subcentimeter mass along the 3 o’clock axis of the left breast, posterior depth. Follow up ultrasound in February of 2008 showed an 8 mm solid mass at 3 o'clock, 9 cm from the nipple, which correlated with the mammographic mass. Ultrasound of the axilla was unremarkable. Biopsy of the mass showed: moderately differentiated invasive ductal carcinoma, grade 2, ER+ (90%), PR+ (50%), her2neu- (1+), Ki-67 10% (low proliferative rate). The patient was referred to surgical oncology, radiation oncology, and medical oncology for consultation; however, she declined any surgical intervention or radiation therapy. Furthermore, the patient stated that she was only willing to take oral therapy, so aromatase inhibitors were thoroughly discussed with the patient including the side effects of osteoporosis. The patient and her daughter voiced understanding and she started Arimidex therapy 1 mg daily in May of 2008.
On initial physical exam no dominant breast mass was palpated and the axillary exam was unremarkable. The 2007 screening mammogram showed (Figures 1-3) a new lobular mass in the along the 3 o’clock axis of the left breast, posterior depth. No additional imaging or intervention was performed and a period of healing was advised given her recent history of multiple right breast interventions.
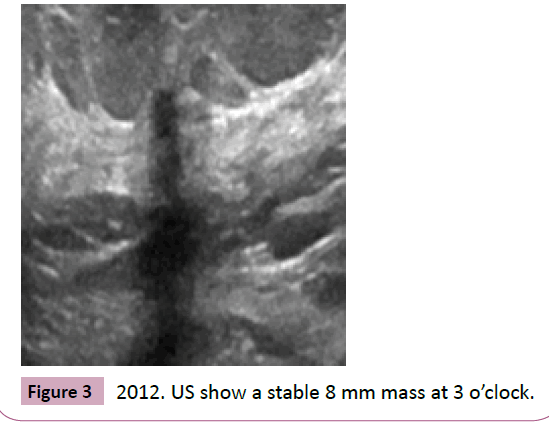
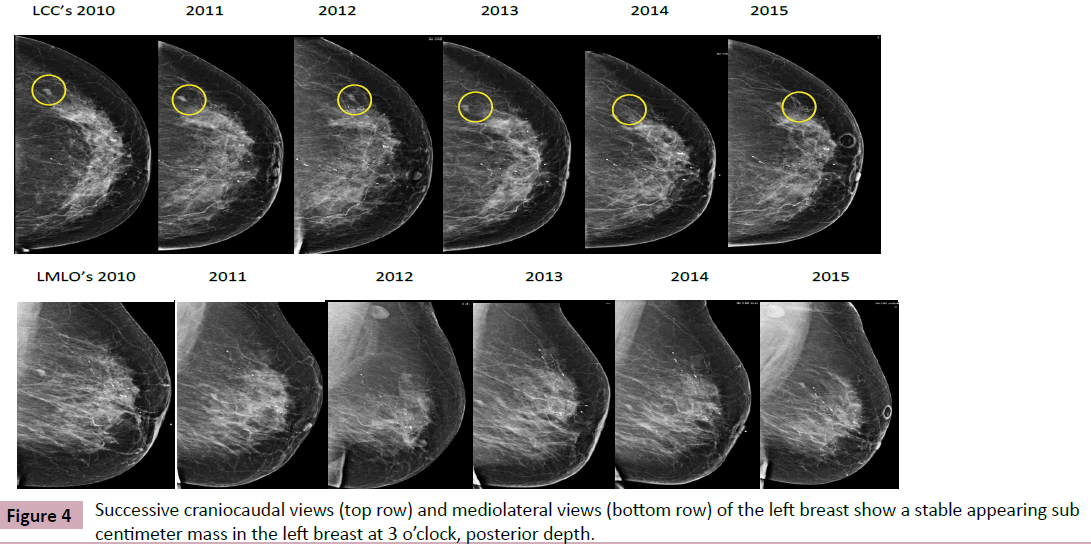
Although the patient declined surgical intervention and radiation therapy, she agreed to annual surveillance mammography to evaluate for tumor progression. Follow up mammograms from 2010-2015 show no mammographic evidence of tumor growth (circled) and the axilla appears stable (Figure 4).
Case 2
A 92 year old G4, P1, A0 female with prior history of left intraductal papilloma and atypical ductal hyperplasia diagnosed in 2002, however excision was not performed due to patient’s comorbidities including CHF, hypertension, atrial fibrillation and coronary artery disease. Other relevant past medical history includes cervical cancer status post hysterectomy (no other therapy per patient), stage I vulvar carcinoma status post local excision, and stage T3, N, and M0 colon adenocarcinoma s/p hemicolectomy.
In August of 2009, the patient presented to an outside facility with a chief complaint of a left breast mass. Mammogram was negative for malignancy, but survey ultrasound demonstrated a 2.1 x 1.1 x 2.1 cm mass at 10 o’clock, 9 cm from the nipple. Core biopsy of the 10 o’clock mass revealed IDC, intermediate grade, ER/PR positive, HER-2/neu negative.
Given the patient’s co-morbidities, the patient was given the choice of (a). Surgical management (total mastectomy), (b). Oral therapy with Arimidex and close imaging follow up, (c) or no intervention. After extensive risk/benefit discussions, the decision was made to proceed with oral daily Arimidex for 3 months with reassessment via ultrasound.
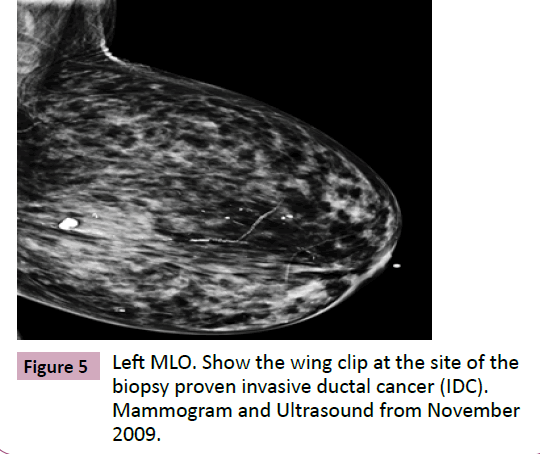
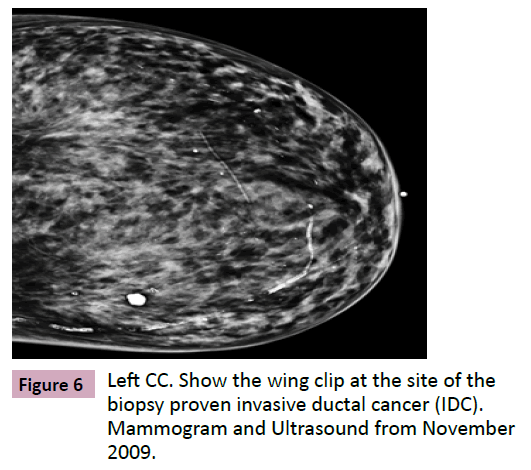
Initial mammogram and ultrasound from August 2009 was not available, however, the follow up ultrasound from the 3 month follow up in November 2009 reveals a 0.6 x 0. 5 x 0.5 cm mass at 10 o’clock, 9 cm from the nipple. This has significantly decreased in size from comparison survey ultrasound in August of 2009 (the reported size in August 2009 was 2.1 x 1.1 x 2.1 cm) (Figures 5 and 6).
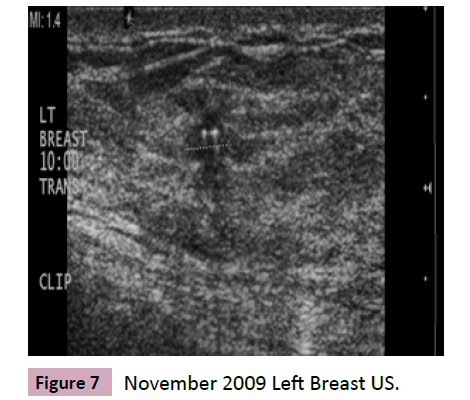
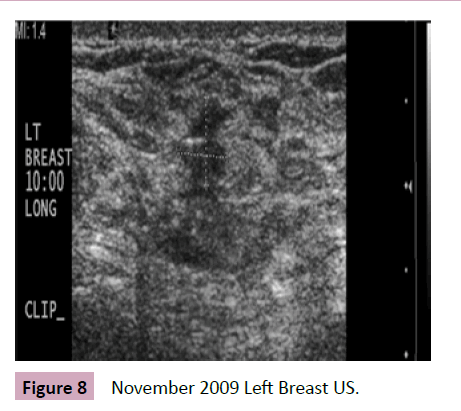
November 2009 ultrasound images show biopsy proven IDC at 10 o’clock, 9 cm from the nipple; correlating with mammographic findings (Figures 7 and 8). The mass measures 0.6 x 0. 5 x 0.5 cm and a post biopsy clip are noted within the mass.
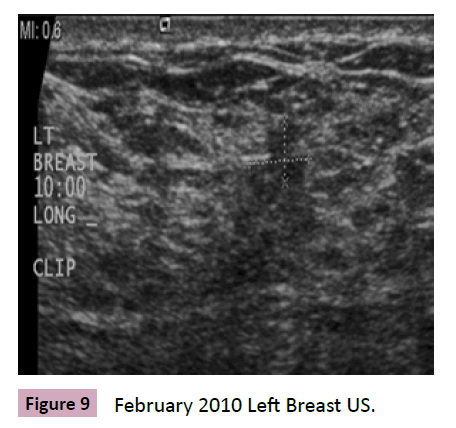
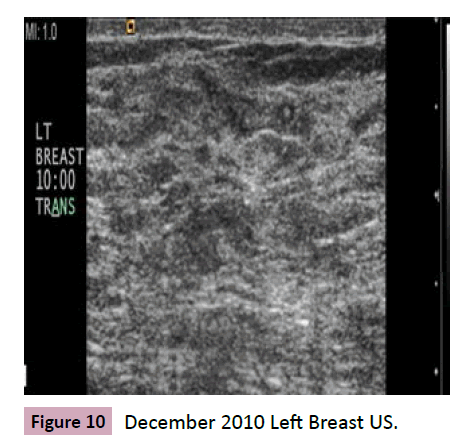
Figure 9 (February 2010) US show that the mass has decreased in size and measures 0.4 x 0.3 x 0.5 cm. Figure 10 (December 2010) shows that the mass is no longer visible by US.
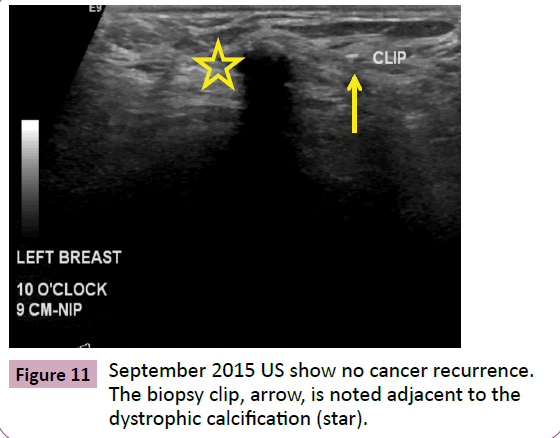
Patient continued annual US surveillance at our institution until September of 2015 at which time she completed 5 years of her oral Arimidex therapy. No recurrence of cancer was noted at this time. Only the clip (arrow) is identified is on the most recent 2015 left breast US, adjacent to the dystrophic calcification (star) (Figure 11).
Discussion
Breast cancer therapy has evolved very quickly over the past decade. We have approached the cancer with more less invasive treatments. The standard of for now is to remove breast cancer with breast conserving surgery when appropriate and then radiate the capsule for small tumors. We consider chemotherapy if the tumor is above one centimeter. We then follow up with 5 to 10 years of hormonal therapy. In post menopausal women greater efficacy has been shown with Aromatase inhibitors [1-8].
These patients have chosen a non standard approach and have lived a normal life for the last seven without many side effects. We use hormonal therapy alone in a great deal of metastatic breast cancer cases with great efficacy. These cases show us that we may be able to spare some elderly postmenopausal women with small tumors surgery, radiation and chemotherapy. The tumor profiles for these cases are perfect for this treatment with it having low KI-67 and high ER percentage. When we put their profile in Adjuvant on line her score was favorable for hormonal therapy [7].
This not standard of care but may be a good choice for elderly post-menopausal women with significant co morbidities or who choose not to have aggressive intervention. In these cases the patients choose not to have surgery, but have been a very compliant patient before the diagnosis of cancer and have been very compliant since. In our present medical model patient want to play a part in determining what therapies are best for them. In some cases we have many choices [9]. Sometimes patients will make choices when there is not much evidence to support their choice and we usually advise against such choices. In these cases the patients have made the right choices.
References
- Napoli A (2013) MR-guided Ultrasound Offers Noninvasive Treatment for Breast Cancer. RSNA Press Release.
- Graham LJ, Shupe MP, Schneble EJ, Flynt FL, Clemenshaw MN, et al. (2014) Current Approaches and Challenges in Monitoring Treatment Responses in Breast Cancer. J Cancer 5: 58–68.
- Zizi-Sermpetzoglou A (2009) Malignant adenomyoepithelioma of the breast--case report. Eur J Gynaecol Oncol 30: 234-236.
- Ahlam A (2012) Malignant Adenomyoepithelioma of the Breast with Lymph Node Metastasis: A Detailed Immunohistochemical Study. Case Reports in Pathology.
- Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, et al. (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years' adjuvant treatment for breast cancer. Lancet 365: 60-62.
- Bonneterre J, Buzdar A, Nabholtz JM, Robertson JF, Thürlimann B, et al. (2001) Anastrozole is superior to tamoxifen as first-line therapy in hormone receptor positive advanced breast carcinoma. Cancer 92: 2247-2258.
- Ravdin PM, Siminoff LA, Davis GJ, Mercer MB, Hewlett J, et al. (2001) Computer Program to Assist in Making Decisions About Adjuvant Therapy for Women With Early Breast Cancer. J Clin Oncol 19: 980-991.
- Goss PE, Ingle JN, Martino S, Robert NJ, Muss HB(2003) A Randomized Trial of Letrozole in Postmenopausal Women after Five Years of Tamoxifen Therapy for Early-Stage Breast Cancer. N Engl J Med 349: 1793-1802.
- Hibbard JH, Peters E(2003) Supporting Informed Consumer Health Care Decisions: Data Presentation Approaches that Facilitate the Use of Information in Choice.Annual Review of Public Health 24: 413-433.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences