Ovarian Adenocarcinoma with Serous Effusions Appeared after a Mammary Adenocarcinoma: A Case Report
Liliana Vecerzan, Romeo-Gabriel Mihaila
DOI10.21767/2572-309X.100004
Liliana Vecerzan1 and Romeo-Gabriel Mihăilă1,2*
1Emergency County Clinical Hospital, Sibiu, Romania
2Lucian Blaga University of Sibiu, Sibiu, Romania
- *Corresponding Author:
- Romeo-Gabriel Mihăilă
Lucian Blaga University of Sibiu
Emergency County Clinical Hospital Sibiu
Sibiu, Romania
Tel: +40269215050
E-mail: romeomihaila@yahoo.com
Received date: December 30, 2015 Accepted date: January 08, 2016 Published date: Januray 25, 2016
Citation: Vecerzan L, Mihăilă RG. Ovarian Adenocarcinoma with Serous Effusions Appeared after a Mammary Adenocarcinoma:A Case Report. J. Adenocarcinoma 2016, 1:1. doi: 10.21767/2572-309X.10004
Abstract
The ovarian adenocarcinoma is an aggressive cancer which has the highest mortality rate of all the gynecological cancers. More than 1/3 of the patients requests medical attention for ascites and pleural effusions. The association of the triad ovarian tumor, ascites and pleural effusions raises diagnostic issues and may lead to delay of adequate treatment. We present the case of a 56 years old female patient, initially diagnosed with bilateral mammary adenocarcinoma, who was treated with chemo- and radiotherapy. Subsequently she developed another adenocarcinoma - this time with ovarian localization. The particularity of this case consists of the risk factors that contributed to the appearance of the ovarian adenocarcinoma with serous effusions, represented by the family and personal history of the patient.
Keywords
Ovarian adenocarcinoma; Mammary adenocarcinoma; Serous effusion
Introduction
Ovarian adenocarcinoma is the most common malignancy of the female genital malignancies and represents one of the principal causes of morbidity and mortality of the females in the world. Its maximal incidence is between 45 and 60 years.
It is most often diagnosed late as the symptomatology is nonspecific, which frequently creates diagnosis difficulties. Most often the ovarian adenocarcinoma is asymptomatic, so at the moment of diagnosis it is already in an advanced stage (FIGO IIIIV) [1,2]. The screening (clinical exam, transvaginal ultrasound or CA125) is useful in the early detection of ovarian cancer in cases with increased risk (family history). Ascites and pleural effusion can have malignant etiology, but it may be difficult to distinguish between metastatic malignant and reactive mesothelial cells present in a serous effusion, as the cells can have similar morphological characteristics. Immunohistochemical study of cell populations is essential for a correct diagnosis and management [3]. Transcriptional factor hepatocyte nuclear factor-1(sup), present in serous effusions, may serve to distinguish between clear cells of serous ovarian carcinoma and those of breast carcinoma. Its role in the differential diagnosis between ovarian carcinomas and adenocarcinomas with another origin is contestable [4].
Ovarian adenocarcinoma has a rapid evolution and has a tendency to relapse even after a radical treatment [1]. The surgical intervention was considered to be useful in the management of this type of cancer for a long period of time. The association between chemo- and radiotherapy may lead to an increased 5 years survival rate, to about 30% [5].
Case Report
An urban, smoker, nulliparous, 56 years old female patient, with known family history of cancer (mother had an ovarian cancer) was diagnosed with right breast adenocarcinoma 10 years ago, for which she had undergone radical mastectomy, followed by chemotherapy (according to the scheme cyclophosphamide 1 g, methotrexate 80 mg, 5-fluorouracil 1 g - 6 cycles) and radiotherapy (at a dose of 50 Gy during 6 weeks). Two years later she was diagnosed with a relapsed disease in the contralateral mammary gland, for which she had also undergone radical mastectomy.
She came in Pulmonology Hospital Sibiu for intense abdominal pain, increased abdominal volume and dry cough in September 2014. On physical examination she was without fever, with decreased vesicular breath sounds basal bilateral, rhythmic heart sounds; her abdomen was increased in volume and sensitive.
Laboratory tests were normal, and the chest X-ray showed bilateral basal pleural effusions, predominantly on the right side, and also increased interstitial markings. The thoracoabdominal CT scan showed bilateral pleural effusions, a retractable area in the right posterior-basal side, and a punctate size pulmonary micro-nodule with a difficult to be established etiology; no pathologic axillary, mediastinal or retrocrural lymph nodes were present; the liver had some hypodense areas with an aspect of hepatic cysts; epigastric and left flank peritoneum appeared to be thickened - aspect suggestive for peritoneal carcinomatosis; a fine perihepatic liquid collection was found. A right thoracentesis was performed and the pleural fluid was serocitrin, Rivaltapositive, with pleural glucose of 65 mg/dL, pleural protein content of 36 mg/dL, lactate dehydrogenase (LDH) of 206 mg/ dL, pleural LDH/serum LDH ratio of 206 mg/dL, negative for Koch bacillus, with tumor cells cytology. She received treatment with antibiotics, diuretics, and hepatoprotective drugs, and the recommendation to be hospitalized in the oncology service for further investigations.
This hospitalization on the Oncology service of the Emergency County Clinical Hospital Sibiu occurred in October 2014, when she had an ECOG performance status of 2, preserved consciousness, anorexia, mat sound in the lung bases with abolished breath sounds, increased abdominal volume due to ascites fluid (shifting dullness), anxiety, oliguria, bilateral post-mastectomy supple scars without signs of recurrence. Laboratory analyzes were in normal limits. The value of tumor markers was: CA 125-9629 U/ mL and CA 15-3-255 U/mL. Repeated thoracoabdominopelvic CT scan showed an increased amount of bilateral pleural effusion (compared to the last examination), with a right posterior-basal retractable area, a stationary punctate size pulmonary micronodule, without pathological axillary, mediastinal or retrocrural lymph nodes; the liver had a stationary CT scan aspect, peritoneum in the epigastric region and left flank was ticked, signifying possible peritoneal metastases; the uterus was inhomogen and the ovaries - slightly increased in size and native homogeneous. The presence of pleural effusions, ascites with tumor cells and the increased value for CA125 were arguments for an ovarian cancer. The first series of polychemotherapy was started with carboplatin (450 mg) and paclitaxel (260 mg), with appropriate premedication and antiemetic protection, tolerated without any incident, followed by further 5 cycles of polychemotherapy, with the same dosage regimen. A partial response was obtained at the end of the treatment. The determination of CA 125 and the control CT scan showed a bilateral very fine residual pleural fluid trace; liver cysts were stationary; the peritoneal thickening was reduced; the uterus and the ovaries were reduced in size compared to the previous examination. Therefore it was decided to go for surgery, given the decrease in the amounts CA 125 and the favorable development of CT scan control. The patient was admitted to the Gynecology service in April 2015, where a total hysterectomy with bilateral oophorectomy was made; in addition - omentectomy with biopsies of diaphragmatic domes and flanks collection. The diagnosis of left ovarian papillary adenocarcinoma with peritoneal dissemination was established at the histopathological examination. After surgery, the evolution was favorable with subsequent normalization of CA 125 values and 3 more courses of chemotherapy were given. On physical examination the patient had an ECOG performance status of 2, anxiety, an abdomen diffusely sensitive on palpation, with increased volume due to the fat storage, and a supple postoperative scarring, with no signs of relapse.
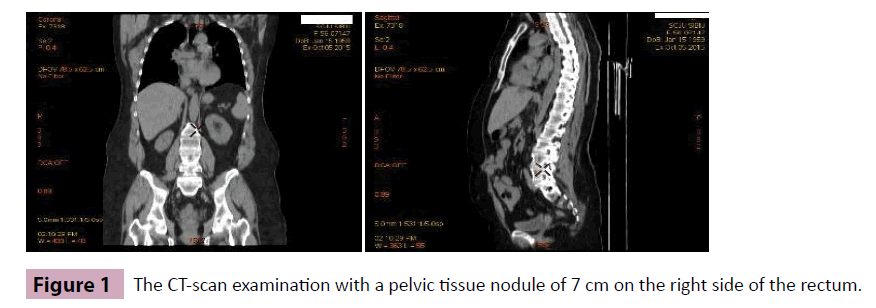
She was hospitalized again in the Oncology service in October 2015, anxiously and depressive, with chest pain, an ECOG performance status of 1, increased abdominal volume due to the fat storage, diffuse and spontaneously sensitive on palpation, sensitive in hypogastric region, postoperative supple scars. The biological tests highlighted an increased value of CA 125 (132.2 U/mL). The CT scan showed: small bilateral pleural effusions, without any condensation in adjacent lungs, and a stationary punctate size pulmonary micro-nodule; no pathological axillary, mediastinal or retrocrural lymph nodes were present; the liver CT scan aspect was stationary; no peritoneal thickening or peritoneal nodules were shown; there was present a pelvic tissue nodule located on the right side of the rectum measuring 7 cm (considered to be a post-hysterectomy tumor recurrence); it was without ascites or retroperitoneal lymphadenopathy (Figure 1).
Abdominal ultrasound examination also found a homogeneous tumor with mixed content, without proper wall at about 3 cm, located near the bladder. The diagnosis of relapsed tumor was established; this was the reason to resume the chemotherapy, with a changed therapeutical scheme.
At the moment, the patient is under the second course of treatment with liposomal doxorubicin, with good gastric tolerance, under antiemetic protection, associated with pain relievers. Her ECOG performance status at discharge was 1.
Discussion
The initial diagnosis was established with some difficulties, as the patient presented pleural effusions and ascites but the ovaries were only slightly enlarged and homogenous at CT scan. The CT scan aspect suggestive for peritoneal carcinoma and the presence of malignant cells in the abdominal fluid were arguments for the presence of a neoplasm. The increased value of CA125 suggested an ovarian neoplasm. The ovarian cancer is characterized by a rapid volume increase and an intra and extra-peritoneal spreading with presence of ascites and pleural effusion. The presence of ascites plays an important role in the progression of the disease and inhibition of chemotherapy response; thus, once appeared, the management of a large quantity of ascites can be a big issue. The patients undergo paracentesis frequently in order to reduce the symptoms [2].
The ovarian adenocarcinoma associated with serous pleural and peritoneal effusions causes problems regarding the positive and differential diagnosis. Most times it is confused with Demons Meigs Syndrome. This syndrome associates a benign tumor with ascites and pleural effusion. The tumor removal leads to serous effusions remission. The marked increase of CA125 associated with Demons Meigs Syndrome is a very rare condition, with few cases reported in the literature. In these situations, the precise diagnosis is made by a histopathological examination [6].
The patient’s mother had an ovarian neoplasm. The existence of an increased risk of ovarian adenocarcinoma was reported in females with a familial history of cancer. The heredity of the ovarian cancer is attributed to mutations in genes BRCA1 and BRCA2; these can be transmitted in an autosomal dominant way to the next generation. BRCA1 and BRCA2 are considered tumor suppressors - they encode proteins with the role of repairing DNA. The mutations of these genes may lead to the loss of their function and produce a genomic instability with a high risk of malignant transformation [7-9].
The coexistence of multiple primary neoplasms is due to a mutation in the glutathione S-transferase gene M1, T1, P1. These encode an important group of enzymes that participate in the xenobiotics metabolism. The members of this subfamily of genes would be involved in the development of multiple cancers [10].
The fact that our patient was treated previously by chemo- and radiotherapy is important. Chemo- and radiotherapy (especially the use of alkylating agents, as to our patient) are considered to be risk factors concerning the appearance of multiple neoplasms. The chemo- and radiotherapy doses, the dimension of irradiated area, and the age of the patient would be involved in the appearance of new cancers – even 10 years after initiation of first treatment; the bigger the doses, the higher the risk [11].
Which are the prognostic factors of patients with ovarian cancer which evolves with serous effusions? This is an important issue as the survival rate at 5 years of patients with such advanced stage ovarian cancer is only 20% [12]. An immuno-histochemical analysis of serous effusions obtained from 143 patients with ovarian cancer found in an advanced stage, treated with chemotherapy based on platinum was made. The effusions were analyzed pre- and post-chemotherapy. In pre-chemotherapy samples, it was shown that survivin (which is an apoptosis inhibitor) was associated with a longer progression free survival, and survivin, signal transducer and activator of transcription 5B, and p21-activated kinase-1 were associated with a longer overall survival. Instead, peroxisome proliferator-activated receptor gamma and human leukocyte antigen-G were associated with a poor progression free survival in patients with post chemotherapy disease recurrence with effusions [13].
How can be managed more efficiently ascites and pleural effusions, outside the classical therapy of ovarian adenocarcinoma? Monoclonal antibodies (as catumaxomab or bevacizumab) and aflibercept (a recombinant fusion protein) were administered intraperitoneally in ascites of patients with ovarian cancers. These medications have shown to reduce the signs and symptoms that accompany ascites, leading to an improved quality of life, increased survival rate and interval between paracentesis [14]. Intrapleural instillations (using a thoracoscope) of a slerotic agent (talcum and doxycycline) were performed for the malignant pleural effusions. This procedure helped to reduce the recurrence of pleural effusion to more than 6 months [15].
Conclusions
The most important risc factor of the ovarian cancer is represented by the presence of an ovarian neoplasm in the patient’s family history. Other following risk factors are mammary neoplasms and nulliparous women.
The tumoral marker CA125, specific to ovarian cancer, is useful for diagnosis and especially for monitoring patient outcomes; an increase of the value of this marker suggests the appearance of local relapse. The surgical intervention, one of the therapeutic tools, is important for the correct histopathological diagnosis establishment and also in choosing appropriate treatment.
The chemo- and radiotherapy used for the treatment of mammary neoplasm of our patient lead to a favorable health evolution in medium term, but in long term they could be considered risk factors for the appearance of this ovarian neoplasm, and maybe other cancers in the future.
References
- Turculeanu A, Balasoiu M, Avramescu C, Danciulescu M, Lungulescu M(2004) Cancerul ovarian - actualitati si perspective. Educatie Medicala Continua.
- Ahmed N,Stenvers KL(2013) Getting to know ovarian cancer ascites: opportunities for targeted therapy-based translational research. Front Oncol3: 256.
- Chowdhuri SR, Fetsch P, Squires J, Kohn E, Filie AC (2014) Adenocarcinoma cells in effusion cytology as a diagnostic pitfall with potential impact on clinical management: a case report with brief review of immunomarkers. Diagn Cytopathol 42: 253-258.
- Davidson B (2014) Hepatocyte nuclear factor-1(sup) is not a specific marker of clear cell carcinoma in serous effusions. Cancer Cytopathol 122: 153-158.
- Popescu-Ilioniu FP (2008) Cancerul ovarian, Ghiduri clinice pentru Obstetrică și Ginecologie, Ghidul 34/Revizia 0.
- Benjapibal M, Sangkarat S, Laiwejpithaya S, Viriyapak B, Chaopotong P, et al.(2009)MeigsSyndromewith elevated serum CA125: Case report and review of the literature. Case Rep Oncol2: 61-66.
- Yang RL, Mick R, Lee K, Graves HL, Nathanson KL, et al. (2015) DCIS inBRCA1andBRCA2mutation carriers: prevalence, phenotype, and expression of oncodrivers C-MET and HER3.J Transl Med 13: 335.
- Pruthi S,Gostout BS, Lindor NM (2010) Identification and management of women withBRCAmutations or hereditary predisposition for breast and ovarian cancer. MDMayo Clin Proc 85: 1111-1120.
- Chiru R, Bujor-Morariu M (2012) Breast cancer – a genetic approach. Revista Practica Medicala 7: 28.
- Chirilã DN, Bãlãcescu O, Popp R (2014) Glutation S-transferazele M1, T1 si P1 la pacientelecu cancere mamare multiple si asocierea cancerului mamar cu un alt tip de cancer.Chirurgia 5: 626-633.
- Berrington de Gonzalez A,Curtis RE,Gilbert E,Berg CD,Smith SA,et al. (2010) Second solid cancers after radiotherapy for breast cancer in SEER cancer registries.Br J Cancer 102: 220-226.
- Miron L (2012) Cancer ovarian. Suport de cursuri pentru rezidenți, Universitatea de Medicină și Farmacie Grigore T Popa Iași.
- Davidson B, Smith Y, Nesland JM, Kærn J, Reich R, et al. (2013) Defining a prognostic marker panel for patients with ovarian serous carcinoma effusion. Hum Pathol 44: 2449-2460.
- Smolle E,Taucher V,Haybaeck J (2014) Malignant ascites in ovarian cancer and the role of targeted therapeutics. Anticancer Res34: 1553-1561.
- Porcel JM, Diaz JP, Chi DS (2012) Clinical implications of pleural effusions in ovarian cancer. Respirology 17: 1060-1067.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences