Correlation of Vascular Endothelial Growth Factor Expression and Neovascularization with Colorectal Carcinoma: A Pilot Study
Hala Abdel Dayem Mohamed, Howyada Sayed Abd El All, Amr Abd El Aziz Kamel, Wagdy Talaat Yossef and Makram Mohamed Hammam
DOI10.21767/2572-309X.100005
Hala Abdel Dayem Mohamed*, Howyada Sayed Abd El All, Amr Abd El Aziz Kamel, Wagdy Talaat Yossef and Makram Mohamed Hammam
Department of Pathology, Faculty of Medicine, Suez Canal University, Ismailia, Egypt
- *Corresponding Author:
- Hala Abdel Dayem Mohamed
Department of Pathology
Faculty of Medicine
Suez Canal University, Ismailia, Egypt
Tel: +9660507161622
E-mail: hala.abdeldayem@yahoo.com
Received date: January 09, 2016; Accepted date: January 19, 2016; Published date: Januray 26, 2016
Citation: Mohamed HAD, Abd El All HS, Kamel AAEA, et al. Correlation of Vascular Endothelial Growth Factor Expression and Neovascularization with Colorectal Carcinoma: A Pilot Study. J. Adenocarcinoma 2016, 1:1. doi: 10.21767/2572-309X.10005
Abstract
Background: In Egypt, there is an increasing incidence of colorectal cancer (CRC), especially among patients under 40 years of age, affecting a very important age group in our community. The basic pathogenic step in the process of tumor growth, invasion and metastasis is tumor induced angiogenesis. The aim of this study was to evaluate the angiogenesis in colorectal carcinoma by detect the expression of VEGF vascular endothelial growth factor and micro vascular density (MVD) determination with IHC (immunohistochemistry) method and to determine if and how angiogenesis correlates with clinicopathologic parameters. Methods and findings: Sixty five archival, paraffin embedded tissue samples of colorectal carcinoma from Pathology Lab of Suez Canal University Teaching Hospital (Egypt) with complete follow-up files in Oncology Unit from. VEGF and micro vessels were identified immunohistochemically, using monoclonal VEGF antibody and CD34 antibody, respectively. VEGF IHC expression was positive in 94.7% of cases and MVD ranged from 9 to 42 mean 24.55 ± 13.79. A significant positive relation was found between VEGF expression; and histological type, tumor grade, lymph node (LN) involvement, UICC TNM classification, perineural and lympho-vascular invasions (p<0.05). A significant positive relation was found between VEGF expression and MVD (p<0.001). There is a significant correlation has been found between MVD and size of the tumor, histological subtype, tumor grade, LN involvement, UICC TNM classification, vascular and perineural invasion and survival (p<0.05). Conclusions: This study has highlighted the prognostic significance of VEGF and MVD to predict survival in CRC patients, as well as some of traditional prognostic factors as tumor histologic type, tumor size, tumor grade, LN involvement, tumor stage and lympho-vascular and perineural invasion to identify patients at high risk for relapse who may benefit from adjuvant treatment including new therapeutic strategies in the future.
Keywords
Colorectal carcinoma; Vascular endothelial growth factor; CD34; Angiogenesis
Introduction
Colorectal cancer is the fourth most common cancer in men and the third most common cancer in women worldwide and significant international variations in the distribution of colorectal cancer have been observed [1], the progressive extension of the Western culture (the essence of "globalization") may lead to a sharp increase in CRC incidence in many countries in the Third World [2].
Tumors stimulate the growth of host blood vessels, a process called angiogenesis, which is essential for supplying nutrients of the tumor. Tumors cannot enlarge beyond 1 to 2 mm in diameter or thickness unless they are vascularized. Beyond this size the tumor fails to enlarge without vascularization because of hypoxia-induced cell death. Angiogenesis is a requisite not only for continued tumor growth but also for metastasis [3].
The development of blood vessels within the tumor mass is regulated by the production of several growth factors and growth inhibitors [4]. In this respect, different growth factors, such as β-transforming growth factor (β -FGF), vascular endothelial growth factor (VEGF) and transforming growth factor-α (TGF- α), have been identified as positive regulators of angiogenesis and are secreted by cancer cells to stimulate normal endothelial cell growth through paracrine mechanisms [5].
Enhanced expression of VEGF has been observed in human cancer cell lines and in cancer patients with different malignancies including colorectal, breast, non-small cell lung and ovarian cancers and is directly correlated with increased neovascularization, as measured by MVD within the tumor [6].
CD34 is a glycosylated type-I trans membrane protein which is expressed on hematopoietic stem cells, committed hematological progenitor cells, small vessel endothelial cells, tumors of epithelial origin and a limited number of other cell populations including some hematological malignancies [7].
Several studies have noted that MVD and expression of VEGF correlates with stage of disease and histological grade of tumor [6,8,9].
In this study, we investigated correlation of the expression of the VEGF and MVD and grade in the tumor tissue of patients with colorectal carcinoma as biological and molecular prognostic factors to identify patients at high risk for relapse who may benefit from adjuvant treatment including new therapeutic strategies in the future.
Patients and Methods
Study population and tumor specimens
The tumor specimens from the patients resected for CRC paraffin blocks were collected from archives of Pathology Laboratory of Suez Canal Teaching Hospital and had complete follow-up files in the Oncology Unit in Suez Canal Teaching Hospital. All the patients were staged according to operative and pathological findings with UICC TNM classification. The clinical and pathological data were collected from medical records, pathology referred report and pathology reports. Follow-up data were obtained from Oncology Unit files. All the patients were observed at least for 36 months after surgery.
The clinical and pathological data included: age, sex, site and size of the tumor, histologic type and grade of the tumor, stage of the patients, surgical margins, lympho-vascular and perineural invasions.
The tumors were categorized according to the (WHO) classification [10]. Histological types of tumors were classical, signet ring and mucinous variants. The grade of classical type tumors (well, moderately and poorly differentiated) was also determined.
Immunohistochemical staining
Briefly, immunostaining was performed using streptavidin-biotin immunoperoxidase complex method with 4-mm thick sections which have been deparaffinized and heated in 0.01 M citrate buffer solution (pH=6) for 15 min for antigen retrieval. For VEGF the slides were boiled in 1mM EDTA, pH 8.0 in a microwave at 1000 w for 5 minutes followed by cooling at room temperature for 20 minutes. Sections were then incubated overnight with anti-VEGF monoclonal antibody AB-1 (Rabbit IgG) (Neomarker).
For CD34 the slides were boiled in the citrate buffer solution pH 6.0 in a microwave at 1000 w for 9 minutes (3 minutes × 3 cycles), followed by cooling at room temperature for 20 minutes. Sections were then incubated overnight with anti- CD34 Ab-1 (endothelial cell marker) (Clone QBEnd/10) (Mouse MAb IgG) (Neomarker). After conjugation with streptavidin-biotin peroxidase complex (broad spectrum LAB-SA detection system, Invitrogen), 3, 3-diaminobenzidine (DAB, Sigma-Aldrich, MO, USA) was used as a chromogen and Mayer’s hematoxylin was used as a counterstain.
Evaluation of VEGF expression
The percentage of positive cells assessed as follows:
Grade 0: 1-5% of positive cells, Grade I: 6-25% of positive cells,
Grade II: 26-50% of positive cells, Grade III: 51-75% of positive cells,
Grade IV: >75% of positive cells. Furthermore, the qualitative intensity of staining for VEGF was assessed as mild, moderate and strong intensity.
Evaluation of CD34 expression
Criteria for vessel counting were those established by Weinder et al. [11]. Any single brown staining endothelial cell or small clusters of brown staining endothelial cells, with or without a lumen were considered as individual vessels. We were blinded to all clinical and pathological data. Slides were examined at low power magnification (40X) to identify the areas of greater concentration of stained vessels "hot spots"; three areas with the highest concentration of micro vessels were selected. Each area was evaluated with one high power (400X) field in such a way as to include the maximum number of micro vessels. The highest value obtained among the three fields was reported for analysis.
Statistical analysis
Results were collected and expressed as the mean ± SD. Results were analyzed using The Statistical Package for the Social Sciences, version 15 (SPSS Software, SPSS Inc., Chicago, USA). Descriptive analysis of data was carried out using the frequencies, mean and median of the relevant data. Relation between the different prognostic and predictive factors was calculated using the Chisquare test. All p-values resulted from two-sided statistical tests and p<0.05 was considered to be significant.
Results
In the current study the expression of VEGF and neovascularization were carried out on 56 cases of CRC patients. The tumor specimens from the patients resected for CRC paraffin blocks were collected from archives of Pathology Laboratory of Suez Canal Teaching Hospital and had complete follow-up files in the Oncology Unit. All the patients were staged according to operative and pathological findings with UICC TNM classification.
The clinical data were collected from medical records and pathology reports. Follow-up data were obtained from Oncology Unit files. All the patients were observed at least 36 months after surgery. All the patients received the same regimen of chemotherapy after the surgery in the Oncology Unit in Suez Canal Teaching Hospital. The main clinicopathological characteristics of our patients are summarized in Table 1. All the patients were observed for at least 36 months after surgery and the 3-years overall survival rate was 33.9% with a median duration 20 months with range (7-36) months, the results of follow up were as showed in Table 1.
| Patients' Characteristics | Total Number (56) | |
|---|---|---|
| Sex | Male | 30 |
| Female | 26 | |
| Age | <40 | 17 |
| 40-60 | 24 | |
| > 60 | 15 | |
| Age range (22-82) years median age of 46.6±4.3 year |
||
| Site | transverse colon | 17 |
| sigmoid | 12 | |
| cecum | 12 | |
| rectum | 6 | |
| descending colon | 5 | |
| ascending colon | 4 | |
| Size | ≥5cm | 35 |
| <5cm | 21 | |
| Tumor size ranged from 2 to 22cm with a mean of 5.02±4.01 | ||
| Histological subtype | well differentiated adenocarcinoma | 11 |
| moderately differentiated adenocarcinoma | 30 | |
| poorly differentiated adenocarcinoma | 4 | |
| mucinous adenocarcinoma | 10 | |
| signet-ring cell carcinoma | 1 | |
| Grade | I | 11 |
| II | 30 | |
| III | 15 | |
| UICC TNM classification | I | 14 |
| II | 26 | |
| III | 16 | |
| lymph nodes metastasis | Positive | 32 |
| Negative | 24 | |
| Surgical margins | Negative | 53 |
| Positive | 3 | |
| Lympho-vascular invasion | Positive | 30 |
| Negative | 26 | |
| Perineural invasion | Positive | 24 |
| Negative | 32 | |
| Survival (months) | <12 | 13 |
| ≥ 12-18> | 14 | |
| ≥18-24> | 6 | |
| ≥ 24-30> | 4 | |
| ≥30-36 | 19 | |
Table 1: Clinicopathologic characteristics of colon cancer cases.
Immunohistochemical staining results
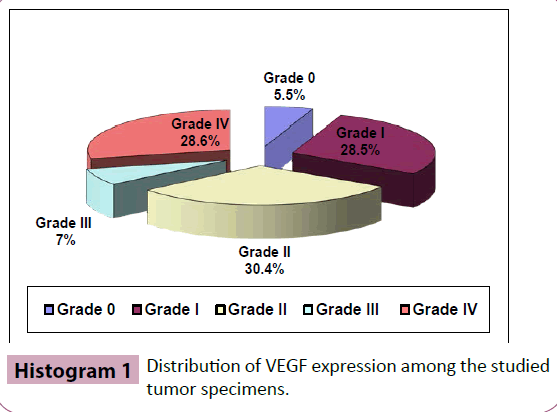
VEGF expression: Positive VEGF was found in 53 cases of 56 patients (94.7%). Positive VEGF immunoreactivity was observed mainly in the cytoplasm of tumor cells. The intensity was moderate in most of cases. The percentage of positive cells assessed as Grade 0, I, II, III and IV. The distribution of VEGF expression among the studied tumor specimens illustrated in Histogram 1. The three negative cases (Grade 0) were all well differentiation adenocarcinoma. VEGF expression was more intense in poorly differentiated adenocarcinoma in comparison to other subtypes (p<0.05).
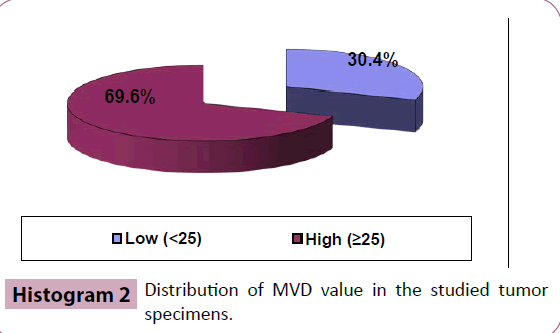
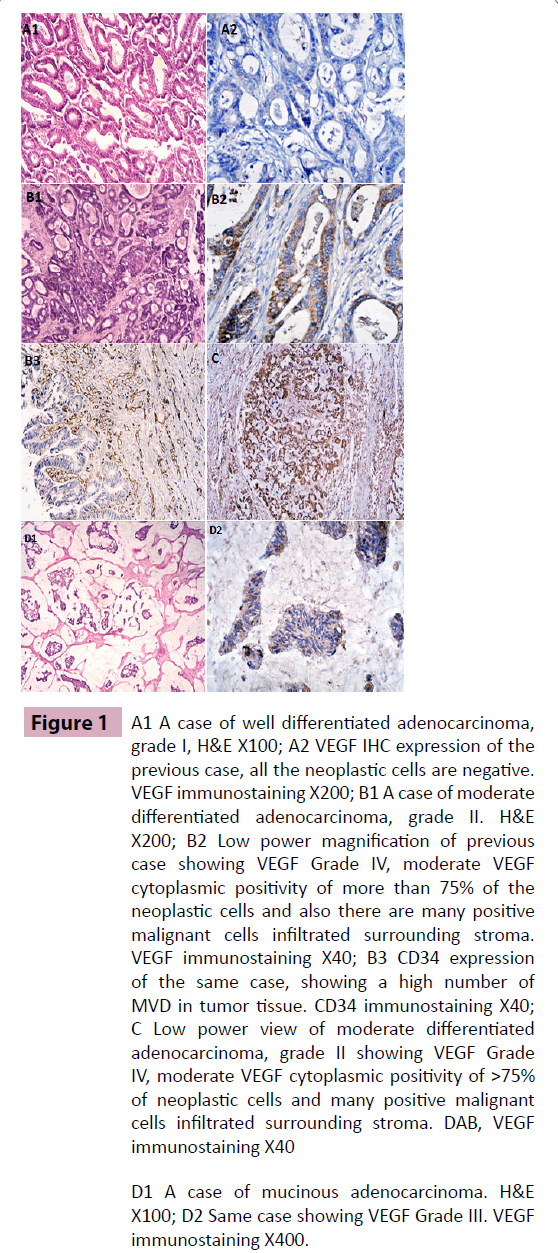
CD34 expression: In the current study, we used CD34 to highlight blood vessels; the size and morphology of vessels were variable. The distribution of angiogenesis in tumor was uneven and heterogeneous. MVD of 56 CRC patients were ranged from 9 to 42 with mean 24.55 ± 13.79. According to the value of MVD, the studied group divided into two groups: low and high; the cutoff point to distinguish low from high was 25, Histogram 2. In some cases MVD was low, while in other cases large vessels were abundant (Figure 1).
VEGF expression and its relation to other clinicopathological parameters
No significant statistical relation has been found between VEGF expression and sex or age of the patients (p>0.05). Also, there is no significant statistical relation has been found between VEGF expression and site and size of the tumor (p>0.05).
A significant positive relation was found between VEGF expression; and histological type, tumor grade, LN involvement, UTCC TNM classification, perineural and lympho-vascular invasions (p<0.05), Table 2.
| Clinico-Pathological Parameter | VEGF EXPRESSION | TOTAL | ||||||
|---|---|---|---|---|---|---|---|---|
| Grade 0 | Grade I | Grade II | Grade III | Grade IV | No.56 | % | ||
| Histological Type | Well diff. | 3 | 5 | 2 | 1 | - | 11 | 19.6 |
| Mod. diff. | - | 10 | 11 | 2 | 7 | 30 | 53.6 | |
| Poorly diff. | - | - | 1 | 1 | 2 | 4 | 7.1 | |
| Mucinous | - | 1 | 2 | - | 7 | 10 | 17.9 | |
| Signet-ring | - | - | 1 | - | - | 1 | 1.8 | |
| Tumor Grade |
I | 3 | 5 | 2 | 1 | - | 11 | 19.6 |
| II | - | 10 | 11 | 2 | 7 | 30 | 53.6 | |
| III | - | 1 | 4 | 1 | 9 | 15 | 26.8 | |
| LN involvement | +ve | - | 1 | 9 | 3 | 11 | 24 | 42.8 |
| -ve | 3 | 15 | 8 | 1 | 5 | 22 | 39.2 | |
| UTCC TNM classification | I | 3 | 7 | 4 | 1 | - | 15 | 26.8 |
| II | - | 9 | 12 | - | 5 | 26 | 46.4 | |
| III | - | - | 1 | 3 | 11 | 15 | 26.8 | |
| Lympho-vascular invasion | -ve | 3 | 14 | 6 | 1 | 2 | 26 | 46.4 |
| +ve | - | 2 | 11 | 3 | 14 | 30 | 53.6 | |
| Perineural invasion | -ve | 3 | 14 | 9 | 1 | 5 | 32 | 57.1 |
| +ve | - | 2 | 8 | 3 | 11 | 24 | 42.9 | |
Table 2: VEGF expression and its relation to clinico-pathological parameters.
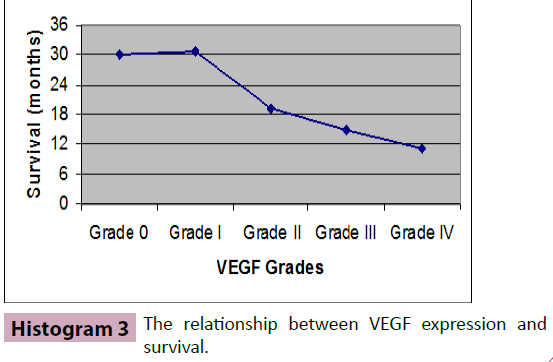
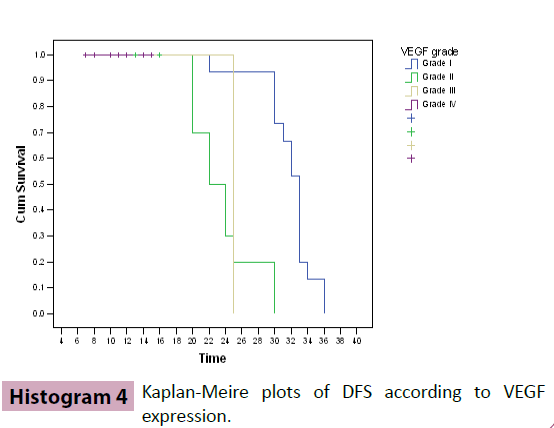
Relationship between VEGF expression and survival showed a positive inverse relation and it was found to be highly statistically significant (p<0.01), Histograms 3 and 4.
Of the 56 cases included in the study 3 cases were negative for VEGF expression (Grade 0), a higher 3-year probability of disease free survival (DFS) was observed in VEGF (Grade 0) patients compared to VEGF positive patients and the difference between the 2 groups was found to be highly statistically significance (p<0.01).
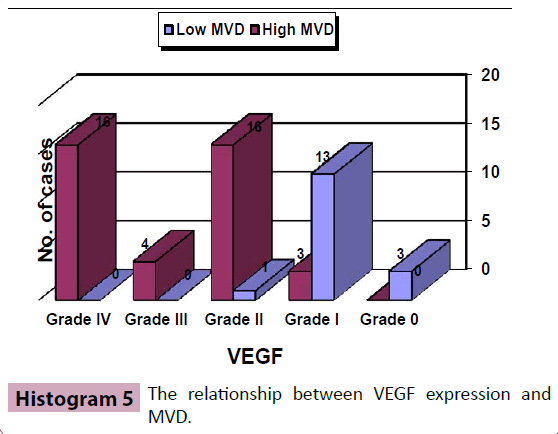
Sixteen cases (28.6%) were VEGF Grade I, 14 cases of all 16 had long survival duration (30-36 months). 17 cases (28.6%) were VEGF Grade II, only 2 of them reached 30 months duration. VEGF Grade III and IV constituted together 20 cases of the whole studied group (35.7%) and 9 cases (45%) of them had survived for duration less than 12 months, another 9 cases had survived for duration between 12 and 18 months, only one case (VEGF Grade III) had survived for 25 months duration, while no case had reached the (30-36) months survival duration. A significant positive relation was found between VEGF expression and MVD (p<0.001), Histogram 5.
MVD determination in CRC specimens and its relation to other clinico-pathological parameters
MVD of 56 CRC patients were ranged from 9 to 42 with mean 24.55 ± 13.79. The size and morphology of vessels were variable. The distribution of angiogenesis in tumor was uneven and heterogeneous. In some cases MVD was very low, while in other cases large vessels were abundant. No significant statistical relation has been found between MVD; and sex or age of the patients (p>0.05). There is a significant correlation has been found between MVD and size of the tumor, histological subtype, tumor grade, LN involvement, UTCC TNM classification, vascular and perineural invasion (p<0.05), Table 3.
| Clinico-Pathological Parameter | MVD | Total | |||
|---|---|---|---|---|---|
| Low(<25) | High(≥25) | No.56 | % | ||
| Size | ≥5cm | 9 | 30 | 39 | 69.6 |
| <5cm | 12 | 5 | 17 | 31.4 | |
| Histological Subtype | Well diff. | 8 | 3 | 11 | 19.6 |
| Mod. diff. | 9 | 21 | 30 | 53.6 | |
| Poorly diff. | - | 4 | 4 | 7.1 | |
| Mucinous | - | 10 | 10 | 17.9 | |
| Signet-ring | - | 1 | 1 | 1.8 | |
| Tumor grade | I | 8 | 3 | 11 | 19.6 |
| II | 9 | 21 | 30 | 53.6 | |
| III | 0 | 15 | 15 | 26.8 | |
| LN involvement | +ve | 0 | 24 | 24 | 42.9 |
| -ve | 17 | 15 | 32 | 57.1 | |
| UTCC TNM classification | I | 8 | 7 | 15 | 26.8 |
| II | 9 | 17 | 26 | 46.4 | |
| III | 0 | 15 | 15 | 26.8 | |
| Lympho-vascular invasion | -ve | 16 | 10 | 26 | 46.4 |
| +ve | 1 | 29 | 30 | 53.6 | |
| Perineural invasion | -ve | 16 | 16 | 32 | 57.1 |
| +ve | 1 | 23 | 24 | 42.9 | |
Table 3: MVD expression and its relation to clinico-pathological parameters.
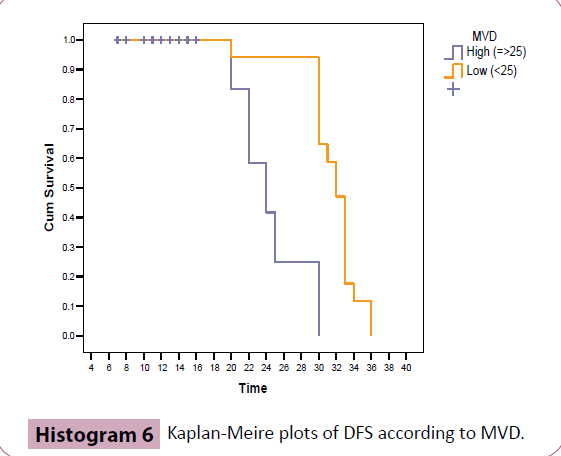
Relationship between MVD and survival showed a positive relation (p<0.05), a higher 3-year probability of disease free survival (DFS) was observed in low MVD patients compared to high MVD patients and the difference between the 2 groups was found to be highly statistically significance (p<0.01), Table 4 and Histogram 6.
| Survival (months) |
MVD | Total | ||
|---|---|---|---|---|
| Low (<25) | High (≥25) | NO. | % | |
| <12 | - | 13 | 13 | 23.2 |
| ≥ 12-18> | - | 14 | 14 | 25 |
| ≥18-24> | 1 | 5 | 6 | 10.7 |
| ≥24-30> | - | 4 | 4 | 7.1 |
| ≥30-36 | 16 | 3 | 19 | 34 |
| Total | 17 | 39 | 56 | 100 |
Table 4: Relation between MVD and survival.
As for relation between survival and other studied prognostic factors a significant positive relations were found between survival and tumor histologic type, primary tumor size, tumor grade, LN involvement, tumor stage, perineural and lymphovascular invasions (p<0.05).
Discussion
In this study IHC was used to characterize the expression of VEGF as a highly specific inducer of angiogenesis and to study the relation between VEGF expression and angiogenesis measured by MVD and the survival in CRC patients.
In the present work 56 cases were eligible for the study, 30 males and 26 females. The age of the patients included in the study ranged from 22 to 82 years with a mean of 49.99 ± 15.7 years. This is consistent with the figures mentioned by Elattar [12], who reported that median age of CRC patients in Egypt is 48 years for both sexes. In the current study 30.4% of patients aged less than 40 years, 42.8% between 40-60 years and 26.8% were aged above 60 years; findings are not very different than those reported by Abdel-Rahman et al. [13] and Abou-Zeid et al. [14].
Soliman et al. [15] and Chan et al. [16] revealed that CRC in Egypt has no age predilection and more than one-third of tumors affect a young population. The high prevalence in young people can neither be explained on a hereditary basis nor can it be attributed to bilharziasis. However, more advanced studies based on molecular analysis concerning this point are lacking in the Egyptian population. Abou-Zeid et al. [14] and Chan et al. [16], speculate that increasing industrialization and urbanization unaccompanied by adequate protective measures contribute to the large bowel cancer problem in Egypt as in many developing countries. The wastes and byproducts of such processes can act as colorectal carcinogens.
Soliman et al. [15] found frighteningly high levels of organochlorine (OC) pesticides in the serum of Egyptian CRC patients. Similarly, other investigators have found that different chemicals and insecticides pollute water and sediments [17-19].
Among the 56 CRC patients for whom follow up data were available; the 3-years overall survival rate was 33.9% with a range of (7-36) months and a median duration 20 months. In the current study, moderate cytoplasmic positivity for VEGF was observed in 53 cases of 56 patients (94.7%). Positive VEGF IHC was observed mainly in the cytoplasm of tumor cells. The intensity was moderate in most of cases. Grade 0 constituted 5.5%, grade I: 28.5%, grade II: 30.4%, grade III: 7% and grade IV: 28.6%.
There was no significant relation between VEGF expression and both sex and age of the patients. These observations do agree with most of other studies [6,20-23] while disagree with Ref. [24] who identified significant relation between VEGF expression and patients’ gender and age.
In our study VEGF appeared to be more expressed in larger tumor size (≥ 5 cm), but there was no significant relation between VEGF expression and size of the tumor, an observation is similar to Zhong et al., Hanrahan et al. and Galizia et al. [21,25,26] and different from other studies where a significant relation was found between the expression of VEGF and primary tumor size [27].
In the current study there was a significant relation between VEGF expression and histologic type of the tumor. VEGF was more expressed in poorly differentiated adenocarcinoma, an observation is similar to Zheng et al. [6]. Among the 56 CRC patients, positive VEGF expression was found in 94.7% of cases. The three negative cases (Grade 0) were all well differentiation adenocarcinoma. VEGF expression was more intense in moderate and poorly differentiated adenocarcinoma in comparison to other well differentiated tumors. A similar observation also reported by other investigators Zheng et al., Jia et al. and Xu et al. [6,22,28].
There was a significant relation between VEGF expression and tumor grade, an observation matching with other studies as van Triest et al. [24] and the Hanrahan et al. [21] who identified that VEGF expression correlated significantly with tumor grade.
In our study, VEGF expression related significantly with LN involvement an observation is agreed with other workers [22,27,29,30].
VEGF expression also related significantly with the tumor stage, in current study we used UICC TNM classification, a result matches with Minagawa et al. [29], Jia et al., Xu et al. [28] and Saumaoro et al. [22,27].
In the present study a significant relation was found between the expression of VEGF and invasion of structures lympho-vascular and perineural invasions an observation previously noted in other works [20,24,27].
In our study, a significant relation was found between VEGF expression and MVD, the same result as Ref. [6,26,31,32].
In the current study VEGF expression was inversely related with prognosis, similarly as the Maeda et al., White et al., Ellis, Galizia et al. and Boxer et al. [26,30-33].
Of the 56 cases included in the study 3 cases were negative for VEGF expression (Grade 0), all these cases had long survival duration between 30 and 36 months. These 3 cases also were all of well differentiated adenocarcinoma type. VEGF Grade I constituted 28.6% of the studied group and 14 cases of all 16 had long survival duration (30-36 months).
VEGF Grade III and IV constituted together 20 cases of the whole studied group (35.7%) and according to duration of survival 9 cases (45%) of them had survived for duration less than 12 months, another 9 cases had survived for duration between 12 and 18 months, only one case (VEGF Grade III) had survived for 25 months duration, while no case had reached the (30-36) months survival duration.
Eleven cases of the patients had VEGF Grade III and IV were under the age of 40 years old (55%) and 6 patients were older than 60 years old. The patient in both age groups had low survival durations (less than 18 months). Of the whole 20 cases had VEGF Grade III and IV, 9 cases (45%) were moderately differentiated adenocarcinoma, 7 cases were mucinous adenocarcinoma, 3 cases were poorly differentiated adenocarcinoma and only one case were well differentiated adenocarcinoma. The small number of poorly differentiated adenocarcinoma and the relatively large number of moderately differentiated adenocarcinoma included in the study may be the cause of this observation.
Fourteen cases had VEGF Grade III and IV was in stage III (UICC TNM classification) and 5 cases were in stage II and the patient in both two stages (II and III) had low survival durations. While only one case was in stage I.
In the present study MVD of 56 CRC patients were ranged from 9 to 42 with mean 24.55 ± 13.79. There was no statistically significant relation between MVD and both age and sex. A similar observation also reported by other investigators [6,26].
There was a significant relation between MVD and size and histologic type of the tumor, an observation is similar to Ref. [6,28]. A significant relation was found between the MVD and tumor grade an observation is matching with the Zheng et al. [6].
Looking for the LN involvement, MVD was significantly related to LN metastasis, this result is the same as the Nakasaki et al. [34] and Xu et al. [28]. MVD also related significantly with the tumor stage (UICC TNM classification) a result matches with Xu et al. [28].
In the present study a significant relation was found between MVD and invasion of structures lympho-vascular and perineurial invasions, an observation is similar to Ref. [35,36].
In this study, MVD was inversely related to survival, an observation is similar to other workers Zheng et al., Ellis, Galizia et al. and Boxer et al. [6,26,31,32]. MVD was significantly higher in tumors that were VEGF-positive than in other tumors a result matches with Maeda et al. [33] and Zheng et al. [6].
As for relation between survival and other studied prognostic factors significant positive relations were found between survival and tumor histologic type, primary tumor size, tumor grade, LN involvement, tumor stage lympho-vascular and perineural invasions. While sex, age, site of primary tumor and lymphovascular and perineural invasions appeared to had no significant positive relations with survival.
As for tumor size, we found that tumor larger than 5 cm had a significant statistical relation with survival; a finding consisted with other investigators [37,38].
In the current study site of primary tumor had no significant statistical relation with survival, same result was reported by Petersen et al. [39]. As a prognostic factor the site of the tumor remains controversial. In one large study, lesions located in the left colon had the most favorable prognosis, whereas those situated in the sigmoid colon and rectum had the worst outcome. In another series, the diagnostic significance of tumor location was found to be minimal [40]. A study with long term followup, showed a greater propensity of left-sided lesions for late recurrences [41].
In the present work histological type of the tumor had a significant statistical relation with survival; a finding is similar to other workers (Assad et al.) [38]. Many investigators reported that mucinous carcinoma, signet ring carcinoma and anaplastic carcinoma have a worse prognosis than the ordinary type of adenocarcinoma, (AJC category IIB) [42].
In the present work tumor grade had a significant statistical relation with survival, a finding that is consisted with (Newland et al.) [37]. Grading of CRCs provides a good key to histological behavior and prognosis. Chapius et al. [43] and Jass et al. [44] found 5-year survival rates of 62% to 83% for grade I, 43% to 63% for grade II and 11% to 42% for grade III.
In the present work LN involvement had a significant statistical relation with survival; a finding is similar to other investigators [37,45]. It has been claimed that once the tumor has spread to the LN, the 5-year survival rate drops sharply (AJC category I). The location and extent of LN involvement are also significant. The greater the number of lymph nodes involved, the worse the prognosis [46,47].
In the present work tumor stage had a significant statistical relation with survival, this result is in agreement with the results of other authors investigating the relation between survival in CRC patients and stage of the tumor using (UICC TNM classification) [22,27,28].
In the present work lympho-vascular and perineural invasions appeared to have a significant statistical relation with survival, a finding is similar to other investigators [24,26,27,48].
Because of the persuasive data demonstrating the importance of VEGF in tumor angiogenesis, an abundance of studies have examined the prognostic value of VEGF expression, tumor vessel count in colon cancer [49]. Using IHC staining of human colon carcinomas, Takahashi et al. [50] observed a significant correlation between the intensity of staining for VEGF and metastatic disease. Also observed that vessel count correlated significantly with expression of VEGF, further implicating these parameters with prognosis. In another study a significant correlation between kinase domain region positive staining endothelial cells and metastatic disease was observed, results of the two studies are supporting the role of VEGF in colorectal cancer progression [51].
VEGF is the driving force behind angiogenesis in most solid malignancies. This also holds true for CRC, where increased levels of VEGF in primary cancers are associated with increased MVD and poor prognosis [26,31,32].
Another important clinical implication beyond prognosis is that VEGF may be a potentially useful target for pharmacologic inhibition of angiogenesis. CRC has been notoriously difficult to treat successfully. Despite numerous attempts at modifying existing therapeutic regimens or designing new ones, survival rates remain low. Nevertheless, studies demonstrate the continued progress that researchers are making in this area and highlight the advances in treatment [52].
Independent experimental studies have shown that it is possible to suppress tumor growth in vivo through inhibition of angiogenesis by blocking the biologic functions of VEGF [53].
Many preclinical studies with anti-angiogenic therapy (anti-VEGF therapy) in colorectal cancer models show that anti-angiogenic therapy can decrease tumor growth, vessel density, angiogenesis, vascular permeability, interstitial pressure and ascites. And also can increase the delivery of chemotherapy and oxygen making radiation therapy more effective. Most importantly, increase survival [54].
Colorectal cancer is the fourth most common cancer in men and the third most common cancer in women worldwide and significant international variations in the distribution of colorectal cancer have been observed [1], the progressive extension of the Western culture (the essence of "globalization") may lead to a sharp increase in CRC incidence in many countries in the Third World [2].
Tumors stimulate the growth of host blood vessels, a process called angiogenesis, which is essential for supplying nutrients of the tumor. Tumors cannot enlarge beyond 1 to 2 mm in diameter or thickness unless they are vascularized. Beyond this size the tumor fails to enlarge without vascularization because of hypoxia-induced cell death. Angiogenesis is a requisite not only for continued tumor growth but also for metastasis [3].
The development of blood vessels within the tumor mass is regulated by the production of several growth factors and growth inhibitors [4]. In this respect, different growth factors, such as β-transforming growth factor (β -FGF), vascular endothelial growth factor (VEGF) and transforming growth factor-α (TGF- α), have been identified as positive regulators of angiogenesis and are secreted by cancer cells to stimulate normal endothelial cell growth through paracrine mechanisms [5].
Enhanced expression of VEGF has been observed in human cancer cell lines and in cancer patients with different malignancies including colorectal, breast, non-small cell lung and ovarian cancers and is directly correlated with increased neovascularization, as measured by MVD within the tumor [6].
CD34 is a glycosylated type-I trans membrane protein which is expressed on hematopoietic stem cells, committed hematological progenitor cells, small vessel endothelial cells, tumors of epithelial origin and a limited number of other cell populations including some hematological malignancies [7].
Several studies have noted that MVD and expression of VEGF correlates with stage of disease and histological grade of tumor [6,8,9].
In this study, we investigated correlation of the expression of the VEGF and MVD and grade in the tumor tissue of patients with colorectal carcinoma as biological and molecular prognostic factors to identify patients at high risk for relapse who may benefit from adjuvant treatment including new therapeutic strategies in the future.
Patients and Methods
Study population and tumor specimens
The tumor specimens from the patients resected for CRC paraffin blocks were collected from archives of Pathology Laboratory of Suez Canal Teaching Hospital and had complete follow-up files in the Oncology Unit in Suez Canal Teaching Hospital. All the patients were staged according to operative and pathological findings with UICC TNM classification. The clinical and pathological data were collected from medical records, pathology referred report and pathology reports. Follow-up data were obtained from Oncology Unit files. All the patients were observed at least for 36 months after surgery.
The clinical and pathological data included: age, sex, site and size of the tumor, histologic type and grade of the tumor, stage of the patients, surgical margins, lympho-vascular and perineural invasions.
The tumors were categorized according to the (WHO) classification [10]. Histological types of tumors were classical, signet ring and mucinous variants. The grade of classical type tumors (well, moderately and poorly differentiated) was also determined.
Immunohistochemical staining
Briefly, immunostaining was performed using streptavidin-biotin immunoperoxidase complex method with 4-mm thick sections which have been deparaffinized and heated in 0.01 M citrate buffer solution (pH=6) for 15 min for antigen retrieval. For VEGF the slides were boiled in 1mM EDTA, pH 8.0 in a microwave at 1000 w for 5 minutes followed by cooling at room temperature for 20 minutes. Sections were then incubated overnight with anti-VEGF monoclonal antibody AB-1 (Rabbit IgG) (Neomarker).
For CD34 the slides were boiled in the citrate buffer solution pH 6.0 in a microwave at 1000 w for 9 minutes (3 minutes × 3 cycles), followed by cooling at room temperature for 20 minutes. Sections were then incubated overnight with anti- CD34 Ab-1 (endothelial cell marker) (Clone QBEnd/10) (Mouse MAb IgG) (Neomarker). After conjugation with streptavidin-biotin peroxidase complex (broad spectrum LAB-SA detection system, Invitrogen), 3, 3-diaminobenzidine (DAB, Sigma-Aldrich, MO, USA) was used as a chromogen and Mayer’s hematoxylin was used as a counterstain.
Evaluation of VEGF expression
The percentage of positive cells assessed as follows:
Grade 0: 1-5% of positive cells, Grade I: 6-25% of positive cells,
Grade II: 26-50% of positive cells, Grade III: 51-75% of positive cells,
Grade IV: >75% of positive cells. Furthermore, the qualitative intensity of staining for VEGF was assessed as mild, moderate and strong intensity.
Evaluation of CD34 expression
Criteria for vessel counting were those established by Weinder et al. [11]. Any single brown staining endothelial cell or small clusters of brown staining endothelial cells, with or without a lumen were considered as individual vessels. We were blinded to all clinical and pathological data. Slides were examined at low power magnification (40X) to identify the areas of greater concentration of stained vessels "hot spots"; three areas with the highest concentration of micro vessels were selected. Each area was evaluated with one high power (400X) field in such a way as to include the maximum number of micro vessels. The highest value obtained among the three fields was reported for analysis.
Statistical analysis
Results were collected and expressed as the mean ± SD. Results were analyzed using The Statistical Package for the Social Sciences, version 15 (SPSS Software, SPSS Inc., Chicago, USA). Descriptive analysis of data was carried out using the frequencies, mean and median of the relevant data. Relation between the different prognostic and predictive factors was calculated using the Chisquare test. All p-values resulted from two-sided statistical tests and p<0.05 was considered to be significant.
Results
In the current study the expression of VEGF and neovascularization were carried out on 56 cases of CRC patients. The tumor specimens from the patients resected for CRC paraffin blocks were collected from archives of Pathology Laboratory of Suez Canal Teaching Hospital and had complete follow-up files in the Oncology Unit. All the patients were staged according to operative and pathological findings with UICC TNM classification.
The clinical data were collected from medical records and pathology reports. Follow-up data were obtained from Oncology Unit files. All the patients were observed at least 36 months after surgery. All the patients received the same regimen of chemotherapy after the surgery in the Oncology Unit in Suez Canal Teaching Hospital. The main clinicopathological characteristics of our patients are summarized in Table 1. All the patients were observed for at least 36 months after surgery and the 3-years overall survival rate was 33.9% with a median duration 20 months with range (7-36) months, the results of follow up were as showed in Table 1.
Immunohistochemical staining results
VEGF expression: Positive VEGF was found in 53 cases of 56 patients (94.7%). Positive VEGF immunoreactivity was observed mainly in the cytoplasm of tumor cells. The intensity was moderate in most of cases. The percentage of positive cells assessed as Grade 0, I, II, III and IV. The distribution of VEGF expression among the studied tumor specimens illustrated in Histogram 1. The three negative cases (Grade 0) were all well differentiation adenocarcinoma. VEGF expression was more intense in poorly differentiated adenocarcinoma in comparison to other subtypes (p<0.05).
5.1.2 CD34 expression: In the current study, we used CD34 to highlight blood vessels; the size and morphology of vessels were variable. The distribution of angiogenesis in tumor was uneven and heterogeneous. MVD of 56 CRC patients were ranged from 9 to 42 with mean 24.55 ± 13.79. According to the value of MVD, the studied group divided into two groups: low and high; the cutoff point to distinguish low from high was 25, Histogram 2. In some cases MVD was low, while in other cases large vessels were abundant (Figure 1).
Figure 1 A1 A case of well differentiated adenocarcinoma, grade I, H&E X100; A2 VEGF IHC expression of the previous case, all the neoplastic cells are negative. VEGF immunostaining X200; B1 A case of moderate differentiated adenocarcinoma, grade II. H&E X200; B2 Low power magnification of previous case showing VEGF Grade IV, moderate VEGF cytoplasmic positivity of more than 75% of the neoplastic cells and also there are many positive malignant cells infiltrated surrounding stroma. VEGF immunostaining X40; B3 CD34 expression of the same case, showing a high number of MVD in tumor tissue. CD34 immunostaining X40; C Low power view of moderate differentiated adenocarcinoma, grade II showing VEGF Grade IV, moderate VEGF cytoplasmic positivity of >75% of neoplastic cells and many positive malignant cells infiltrated surrounding stroma. DAB, VEGF immunostaining X40
D1 A case of mucinous adenocarcinoma. H&E X100; D2 Same case showing VEGF Grade III. VEGF immunostaining X400.
VEGF expression and its relation to other clinicopathological parameters
No significant statistical relation has been found between VEGF expression and sex or age of the patients (p>0.05). Also, there is no significant statistical relation has been found between VEGF expression and site and size of the tumor (p>0.05).
A significant positive relation was found between VEGF expression; and histological type, tumor grade, LN involvement, UTCC TNM classification, perineural and lympho-vascular invasions (p<0.05), Table 2.
Relationship between VEGF expression and survival showed a positive inverse relation and it was found to be highly statistically significant (p<0.01), Histograms 3 and 4.
Of the 56 cases included in the study 3 cases were negative for VEGF expression (Grade 0), a higher 3-year probability of disease free survival (DFS) was observed in VEGF (Grade 0) patients compared to VEGF positive patients and the difference between the 2 groups was found to be highly statistically significance (p<0.01).
Sixteen cases (28.6%) were VEGF Grade I, 14 cases of all 16 had long survival duration (30-36 months). 17 cases (28.6%) were VEGF Grade II, only 2 of them reached 30 months duration. VEGF Grade III and IV constituted together 20 cases of the whole studied group (35.7%) and 9 cases (45%) of them had survived for duration less than 12 months, another 9 cases had survived for duration between 12 and 18 months, only one case (VEGF Grade III) had survived for 25 months duration, while no case had reached the (30-36) months survival duration. A significant positive relation was found between VEGF expression and MVD (p<0.001), Histogram 5.
MVD determination in CRC specimens and its relation to other clinico-pathological parameters
MVD of 56 CRC patients were ranged from 9 to 42 with mean 24.55 ± 13.79. The size and morphology of vessels were variable. The distribution of angiogenesis in tumor was uneven and heterogeneous. In some cases MVD was very low, while in other cases large vessels were abundant. No significant statistical relation has been found between MVD; and sex or age of the patients (p>0.05). There is a significant correlation has been found between MVD and size of the tumor, histological subtype, tumor grade, LN involvement, UTCC TNM classification, vascular and perineural invasion (p<0.05), Table 3.
Relationship between MVD and survival showed a positive relation (p<0.05), a higher 3-year probability of disease free survival (DFS) was observed in low MVD patients compared to high MVD patients and the difference between the 2 groups was found to be highly statistically significance (p<0.01), Table 4 and Histogram 6.
As for relation between survival and other studied prognostic factors a significant positive relations were found between survival and tumor histologic type, primary tumor size, tumor grade, LN involvement, tumor stage, perineural and lymphovascular invasions (p<0.05).
Discussion
In this study IHC was used to characterize the expression of VEGF as a highly specific inducer of angiogenesis and to study the relation between VEGF expression and angiogenesis measured by MVD and the survival in CRC patients.
In the present work 56 cases were eligible for the study, 30 males and 26 females. The age of the patients included in the study ranged from 22 to 82 years with a mean of 49.99 ± 15.7 years. This is consistent with the figures mentioned by Elattar [12], who reported that median age of CRC patients in Egypt is 48 years for both sexes. In the current study 30.4% of patients aged less than 40 years, 42.8% between 40-60 years and 26.8% were aged above 60 years; findings are not very different than those reported by Abdel-Rahman et al. [13] and Abou-Zeid et al. [14].
Soliman et al. [15] and Chan et al. [16] revealed that CRC in Egypt has no age predilection and more than one-third of tumors affect a young population. The high prevalence in young people can neither be explained on a hereditary basis nor can it be attributed to bilharziasis. However, more advanced studies based on molecular analysis concerning this point are lacking in the Egyptian population. Abou-Zeid et al. [14] and Chan et al. [16], speculate that increasing industrialization and urbanization unaccompanied by adequate protective measures contribute to the large bowel cancer problem in Egypt as in many developing countries. The wastes and byproducts of such processes can act as colorectal carcinogens.
Soliman et al. [15] found frighteningly high levels of organochlorine (OC) pesticides in the serum of Egyptian CRC patients. Similarly, other investigators have found that different chemicals and insecticides pollute water and sediments [17-19].
Among the 56 CRC patients for whom follow up data were available; the 3-years overall survival rate was 33.9% with a range of (7-36) months and a median duration 20 months. In the current study, moderate cytoplasmic positivity for VEGF was observed in 53 cases of 56 patients (94.7%). Positive VEGF IHC was observed mainly in the cytoplasm of tumor cells. The intensity was moderate in most of cases. Grade 0 constituted 5.5%, grade I: 28.5%, grade II: 30.4%, grade III: 7% and grade IV: 28.6%.
There was no significant relation between VEGF expression and both sex and age of the patients. These observations do agree with most of other studies [6,20-23] while disagree with Ref. [24] who identified significant relation between VEGF expression and patients’ gender and age.
In our study VEGF appeared to be more expressed in larger tumor size (≥ 5 cm), but there was no significant relation between VEGF expression and size of the tumor, an observation is similar to Zhong et al., Hanrahan et al. and Galizia et al. [21,25,26] and different from other studies where a significant relation was found between the expression of VEGF and primary tumor size [27].
In the current study there was a significant relation between VEGF expression and histologic type of the tumor. VEGF was more expressed in poorly differentiated adenocarcinoma, an observation is similar to Zheng et al. [6]. Among the 56 CRC patients, positive VEGF expression was found in 94.7% of cases. The three negative cases (Grade 0) were all well differentiation adenocarcinoma. VEGF expression was more intense in moderate and poorly differentiated adenocarcinoma in comparison to other well differentiated tumors. A similar observation also reported by other investigators Zheng et al., Jia et al. and Xu et al. [6,22,28].
There was a significant relation between VEGF expression and tumor grade, an observation matching with other studies as van Triest et al. [24] and the Hanrahan et al. [21] who identified that VEGF expression correlated significantly with tumor grade.
In our study, VEGF expression related significantly with LN involvement an observation is agreed with other workers [22,27,29,30].
VEGF expression also related significantly with the tumor stage, in current study we used UICC TNM classification, a result matches with Minagawa et al. [29], Jia et al., Xu et al. [28] and Saumaoro et al. [22,27].
In the present study a significant relation was found between the expression of VEGF and invasion of structures lympho-vascular and perineural invasions an observation previously noted in other works [20,24,27].
In our study, a significant relation was found between VEGF expression and MVD, the same result as Ref. [6,26,31,32].
In the current study VEGF expression was inversely related with prognosis, similarly as the Maeda et al., White et al., Ellis, Galizia et al. and Boxer et al. [26,30-33].
Of the 56 cases included in the study 3 cases were negative for VEGF expression (Grade 0), all these cases had long survival duration between 30 and 36 months. These 3 cases also were all of well differentiated adenocarcinoma type. VEGF Grade I constituted 28.6% of the studied group and 14 cases of all 16 had long survival duration (30-36 months).
VEGF Grade III and IV constituted together 20 cases of the whole studied group (35.7%) and according to duration of survival 9 cases (45%) of them had survived for duration less than 12 months, another 9 cases had survived for duration between 12 and 18 months, only one case (VEGF Grade III) had survived for 25 months duration, while no case had reached the (30-36) months survival duration.
Eleven cases of the patients had VEGF Grade III and IV were under the age of 40 years old (55%) and 6 patients were older than 60 years old. The patient in both age groups had low survival durations (less than 18 months). Of the whole 20 cases had VEGF Grade III and IV, 9 cases (45%) were moderately differentiated adenocarcinoma, 7 cases were mucinous adenocarcinoma, 3 cases were poorly differentiated adenocarcinoma and only one case were well differentiated adenocarcinoma. The small number of poorly differentiated adenocarcinoma and the relatively large number of moderately differentiated adenocarcinoma included in the study may be the cause of this observation.
Fourteen cases had VEGF Grade III and IV was in stage III (UICC TNM classification) and 5 cases were in stage II and the patient in both two stages (II and III) had low survival durations. While only one case was in stage I.
In the present study MVD of 56 CRC patients were ranged from 9 to 42 with mean 24.55 ± 13.79. There was no statistically significant relation between MVD and both age and sex. A similar observation also reported by other investigators [6,26].
There was a significant relation between MVD and size and histologic type of the tumor, an observation is similar to Ref. [6,28]. A significant relation was found between the MVD and tumor grade an observation is matching with the Zheng et al. [6].
Looking for the LN involvement, MVD was significantly related to LN metastasis, this result is the same as the Nakasaki et al. [34] and Xu et al. [28]. MVD also related significantly with the tumor stage (UICC TNM classification) a result matches with Xu et al. [28].
In the present study a significant relation was found between MVD and invasion of structures lympho-vascular and perineurial invasions, an observation is similar to Ref. [35,36].
In this study, MVD was inversely related to survival, an observation is similar to other workers Zheng et al., Ellis, Galizia et al. and Boxer et al. [6,26,31,32]. MVD was significantly higher in tumors that were VEGF-positive than in other tumors a result matches with Maeda et al. [33] and Zheng et al. [6].
As for relation between survival and other studied prognostic factors significant positive relations were found between survival and tumor histologic type, primary tumor size, tumor grade, LN involvement, tumor stage lympho-vascular and perineural invasions. While sex, age, site of primary tumor and lymphovascular and perineural invasions appeared to had no significant positive relations with survival.
As for tumor size, we found that tumor larger than 5 cm had a significant statistical relation with survival; a finding consisted with other investigators [37,38].
In the current study site of primary tumor had no significant statistical relation with survival, same result was reported by Petersen et al. [39]. As a prognostic factor the site of the tumor remains controversial. In one large study, lesions located in the left colon had the most favorable prognosis, whereas those situated in the sigmoid colon and rectum had the worst outcome. In another series, the diagnostic significance of tumor location was found to be minimal [40]. A study with long term followup, showed a greater propensity of left-sided lesions for late recurrences [41].
In the present work histological type of the tumor had a significant statistical relation with survival; a finding is similar to other workers (Assad et al.) [38]. Many investigators reported that mucinous carcinoma, signet ring carcinoma and anaplastic carcinoma have a worse prognosis than the ordinary type of adenocarcinoma, (AJC category IIB) [42].
In the present work tumor grade had a significant statistical relation with survival, a finding that is consisted with (Newland et al.) [37]. Grading of CRCs provides a good key to histological behavior and prognosis. Chapius et al. [43] and Jass et al. [44] found 5-year survival rates of 62% to 83% for grade I, 43% to 63% for grade II and 11% to 42% for grade III.
In the present work LN involvement had a significant statistical relation with survival; a finding is similar to other investigators [37,45]. It has been claimed that once the tumor has spread to the LN, the 5-year survival rate drops sharply (AJC category I). The location and extent of LN involvement are also significant. The greater the number of lymph nodes involved, the worse the prognosis [46,47].
In the present work tumor stage had a significant statistical relation with survival, this result is in agreement with the results of other authors investigating the relation between survival in CRC patients and stage of the tumor using (UICC TNM classification) [22,27,28].
In the present work lympho-vascular and perineural invasions appeared to have a significant statistical relation with survival, a finding is similar to other investigators [24,26,27,48].
Because of the persuasive data demonstrating the importance of VEGF in tumor angiogenesis, an abundance of studies have examined the prognostic value of VEGF expression, tumor vessel count in colon cancer [49]. Using IHC staining of human colon carcinomas, Takahashi et al. [50] observed a significant correlation between the intensity of staining for VEGF and metastatic disease. Also observed that vessel count correlated significantly with expression of VEGF, further implicating these parameters with prognosis. In another study a significant correlation between kinase domain region positive staining endothelial cells and metastatic disease was observed, results of the two studies are supporting the role of VEGF in colorectal cancer progression [51].
VEGF is the driving force behind angiogenesis in most solid malignancies. This also holds true for CRC, where increased levels of VEGF in primary cancers are associated with increased MVD and poor prognosis [26,31,32].
Another important clinical implication beyond prognosis is that VEGF may be a potentially useful target for pharmacologic inhibition of angiogenesis. CRC has been notoriously difficult to treat successfully. Despite numerous attempts at modifying existing therapeutic regimens or designing new ones, survival rates remain low. Nevertheless, studies demonstrate the continued progress that researchers are making in this area and highlight the advances in treatment [52].
Independent experimental studies have shown that it is possible to suppress tumor growth in vivo through inhibition of angiogenesis by blocking the biologic functions of VEGF [53].
Many preclinical studies with anti-angiogenic therapy (anti-VEGF therapy) in colorectal cancer models show that anti-angiogenic therapy can decrease tumor growth, vessel density, angiogenesis, vascular permeability, interstitial pressure and ascites. And also can increase the delivery of chemotherapy and oxygen making radiation therapy more effective. Most importantly, increase survival [54].
References
- Center MM, Jemal A, Ward E (2009) International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomarkers Prev 18: 1688-1694.
- Ponz de Leon M, Benatti P, Borghi F, Pedroni M, Scarselli A, et al. (2004) Aetiology of colorectal cancer and relevance of monogenic inheritance. Gut 53: 115-22.
- Kerbel RS (2000) Tumor angiogenesis: past, present and the near future. Carcinogenesis 21: 505-515.
- Klagsbrun M, D’Amore PA (1991) Regulation of angiogenesis. Annu Rev Physiol 53: 217-39.
- Ciardiello F, Bianco R, Damiano V, Fontanini G, Caputo R, et al. (2000) Antiangiogenic and antitumor activity of anti-epidermal growth factor receptor C225 monoclonal antibody in combination with vascular endothelial growth factor antisense oligonucleotide in human GEO colon cancer cells. Clin Canc Res 6: 3739-3747.
- Zheng S, Han MY, Xiao ZX, Peng JP, Dong Q (2003) Clinical significance of vascular endothelial growth factor expression and neovascularization in colorectal carcinoma. World J Gastroenterol 9: 1227-1230.
- Lanza F, Healy L, Sutherland DR (2001) Structural and functional features of the CD34 antigen. J Biol Regul Homeost Agents 15: 1-13.
- Fenjvesi A (2003) Prognostic significance of tumor-induced angiogenesis in colorectal carcinoma. Med Pregl 56: 263-268.
- Cristi E, Perrone G, Toscano G, Verzì A, Nori S, et al. (2005) Tumour proliferation, angiogenesis, and ploidy status in human colon cancer. J Clin Pathol 58: 1170-1174.
- Jass JR, Sobin LH (1989) Histological typing of intestinal tumors. World Health Organization International Histological Classification of Tumors. 2nd (edn), New York: Spring-Verlag.
- Weidner N, Folkman J, Pozza F, Bevilacqua P, Allred EN, et al. (1992) Tumor angiogenesis: a new significant and independent prognostic indicator in early-stage breast carcinoma. J Natl Cancer Inst 84: 1875-1887.
- Elattar I (2005) Annual Cancer Conference of the Egyptian Cancer Society, Danish Cancer Society & Aarhus University Hospital.
- Abdel-Rahman SZ, Soliman AS, Bondy ML, Wu X, El-Badawy SA, et al. (1999) Polymorphism of glutathione S-transferase loci GSTM1 and GSTT1 and susceptibility to colorectal cancer in Egypt. Cancer Lett 142: 97-104.
- Abou-Zeid AA, Khafagy W, Marzouk DM, Alaa A, Mostafa I, et al. (2002) Colorectal cancer in Egypt. Diseases of the Colon & Rectum 45: 1255-1260.
- Soliman AS, Bondy ML, El-Badawy SA, Mokhtar N, Eissa S, et al. (2001) Contrasting molecular pathology of colorectal carcinoma in Egyptian and Western patients. Br J Cancer 85: 1037-1046.
- Chan AO, Soliman AS, Zhang Q, Rashid A, Bedeir A, et al. (2005) Differing DNA methylation patterns and gene mutation frequencies in colorectal carcinomas from middle eastern countries. Clin Cancer Res 11: 8281-8287.
- El-Gendy KS, Abdalla AA, Aly HA, Tantawy G, El-Sebae AH (1991) Residue levels of chlorinated hydrocarbon compounds in water and sediment samples from Nile branches in the delta, Egypt. J Environ Sci Health 26: 15-36.
- Badawy MI, Wahaab RA, Abou Waly HF (1995) Petroleum and chlorinated hydrocarbons in water from lake Manzala and associated canals. Bull Environ Contam Toxicol 55: 258-263.
- Howsam M, Grimalt JO, Guino E, Navarro M, Marti-Rague J, et al. (2004) Organochlorine exposure and colorectal cancer risk. Environ Health Perspect 112: 1460-1466.
- Akagi K, Ikeda Y, Miyazaki M, Abe T, Kinoshita J, et al. (2000) Vascular endothelial growth factor-C (VEGF-C) expression in human colorectal cancer tissues. Br J Cancer 83: 887-891.
- Hanrahan V, Currie MJ, Gunningham SP, Morrin HR, Scott PA, et al. (2003) The angiogenic switch for vascular endothelial growth factor VEGF-A, VEGF-B, VEGF-C and VEGF-D in the adenoma-carcinoma sequence during colorectal cancer progression. J Pathol 2: 183-194.
- Jia Y-T, Li Z-X, He Y-T, Liang W, Yang H-C, Ma HJ (2004) Expression of vascular endothelial growth factor-C and the relationship between lymphangiogenesis and lymphatic metastasis in colorectal cancer. World J Gastroenterol 10: 3261-3263.
- Xu T, Chen D, Chen J (2004) Expression of vascular endothelial growth factor C and its correlation with lymph node metastasis in colorectal carcinoma. J Huazhong Univ Sci Technolog Med Sci 24: 596-598.
- van Triest B, Pinedo HM, Blaauwgeers JL, van Diest PJ, Schoenmakers PS, et al. (2000) Prognostic role of thymidylate synthase, thymidine phosphorylase/platelet-derived endothelial cell growth factor and proliferation markers in colorectal Cancer. Clin Cancer Res 6: 1063-1072.
- Zhong S, Zhang Z, Li S (2001) Significance of vascular endothelial growth factor expression in colorectal cancer. World J Gastroenterol 40: 514-516.
- Galizia G, Lieto E, Ferraraccio F, Orditura M, De Vita F, et al. (2004) Determination of molecular marker expression can predict clinical outcome in colon carcinomas. Clin Cancer Res 10: 3490-3499.
- Saumaoro LT, Uetake H, Takagi Y, Iida S, Higuchi T, et al. (2006) Coexpression of VEGF-C and Cox-2 in human colorectal cancer and its association with lymph node metastasis. Dis Colon Rectum 49: 392-398.
- Xu Q, Chen RX, Wang ZW, Ni QC, Qian JJ, et al. (2005) Clinical research on angiogenesis in colorectal carcinoma and expression of CK20 mRNA in peripheral blood. Zhonghua Yi Xue Za Zhi 85: 1205-1208.
- Minagawa N, Nakayama Y, Hirata K, Onitsuka K, Inoue Y, et al. (2002) Correlation of plasma level and immunohistochemical expression of vascular endothelial growth factor in patients with advanced colorectal cancer. Anticancer Res 22: 2957-2963.
- White JD, Hewett PW, Kosuge D, McCulloch T, Enholm BC, et al. (2002) Vascular endothelial growth factor-D expression is an independent prognostic marker for survival in colorectal carcinoma. Cancer Research 62: 1669-1675.
- Ellis LM (2004) Preclinical data targeting vascular endothelial growth factor in colorectal cancer. Clin Colorectal Cancer 4: 55-61.
- Boxer GM, Tsiompanou E, Levine T, Watson R, Begent RH (2005) Immunohistochemical expression of vascular endothelial growth factor and micro vessel counting as prognostic indicators in node-negative colorectal cancer. Tumour Biol 26: 1-8.
- Maeda K, Nishiguchi Y, Yashiro M, Yamada S, Onoda N, et al. (2000) Expression of vascular endothelial growth factor and thrombospondin-1 in colorectal carcinoma. Int J Mol Med 5: 373-378.
- Nakasaki T, Wada H, Shigemori C, Miki C, Gabazza EC, et al. (2002) Expression of tissue factor and vascular endothelial growth factor is associated with angiogenesis in colorectal cancer. Am J Hematol 69: 247-254.
- Garcea G, Lloyd TD, Gescher A, Dennison AR, Steward WP, et al. (2004) Angiogenesis of gastrointestinal tumours and their metastases–a target for intervention? Eur J Cancer 40: 1302-1313.
- Wali RK, Roy HK, Kim YL, Liu Y, Koetsier JL, et al. (2005) Increased microvascular blood content is an early event in colon carcinogenesis. Gut 54: 654-660.
- Newland RC, Dent OF, Lyttle MN, Chapuis PH, Bokey EL (1994) Pathologic determinants of survival associated with colorectal cancer with lymph node metastases. Cancer 15: 2076-2082.
- Assad NY, Kandil MA, Mokhtar NM (2000) Prognostic value of cyclin D1 and p53 protein in colorectal carcinoma. J Egypt Natl Cancer Inst 12: 283-292.
- Petersen VC, Baxter KJ, Love SB, Shepherd NA (2002) Identification of objective pathological prognostic determinants and models of prognosis in Dukes' B colon cancer. Gut 51: 65-69.
- Steinberg SM, Bakin JS, Kaplan RS, Stablein DM (1986) Prognostic indicators of colon indicators of colon tumors. The Gastrointestinal Tumor Study Group experience. Cancer 57: 1866-1870.
- Eisenberg B, De Cosse JJ, Harford F, Michalack J (1982) Carcinoma of the colon and rectum. The natural history reviewed in 1704 patients’ cancer. Cancer 94: 1131-1134.
- Whittaker MA, Carr NJ, Midwinter MJ, Badham DP, Higgins B (2000) Acinar morphology in colorectal cancer is associated with survival but is not an independent prognostic variable. Histopathology 36: 439-442.
- Chapius PH, Deut OF, Fisher R (1985) A multivariate analysis of clinical and pathological variables in prognosis after resection of large bowel cancer. Br J Surg 72: 698-703.
- Jass JR, Atkin WS, Guzick J, Bussey HJR, Morson BC, et al. (1986) The grading of rectal cancer: Historical perspective and multivariant analysis of 447 cases. Histopathol 10: 437-439.
- Wong JH, Severino R, Honnebier MB, Tom P, Namiki TS (1999) Number of nodes examined and staging accuracy in colorectal carcinoma. J Clin Oncology 9: 2896-2899.
- Liefers GJ, Cleton-Jansen AM, van de Velde CJ, Hermans J, van Krieken JH, et al. (1998) Micrometastases and survival in stage II colorectal cancer. N Engl Med 339: 223-228.
- Stocchi L, Nelson H, Sargent DJ, O’Connell MJ, Tepper JE, et al. (2001) Impact of surgical and pathologic variables in rectal cancer: A United States community and cooperative group report. J Clinl Oncol 18: 3895-3902.
- Compton CC (2003) Colorectal carcinoma: diagnostic, prognostic and molecular features. Mod Pathol 16: 376-388.
- Boige V, Malka D, Ducreux M (2005) Therapeutic strategies using VEGF inhibitors in colorectal cancer. Bull Cancer 92: 29-36.
- Takahashi Y, Tucker SL, Kitadai Y, Koura AN, Bucana CD, et al. (1997) Vessel counts and expression of vascular endothelial growth factor as prognostic factors in node-negative colon cancer. Arch Surg 132: 541-546.
- Takahashi Y, Kitadai Y, Bucana CD, Cleary KR , Ellis LM (1995) Expression of vascular endothelial growth factor and its receptor, KDR, correlates with vascularity, metastasis and proliferation of human colon cancer. Cancer Res 55: 3964-3968.
- Berlin JD, Lockhart C (2002) Treatment of colorectal cancer: An overview of the latest data. Program and abstracts of the American Society of Clinical Oncology 38th Annual Meeting; May 18-21, 2002. Orlando, Florida, USA. Medscape Oncology Abstract. p: 511.
- Rosen LS (2005) VEGF-targeted therapy: Therapeutic potential and recent advances. The Oncologist 6: 382-391.
- Pradeep CR, Sunila ES, Kuttan G (2005) Expression of vascular endothelial growth factor and VEGF receptors in tumor angiogenesis and malignancies. Integrative Cancer Therapies 4: 315-321.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences